Neurodiversity Affirming Practice for Mental Health
In 2024 I delivered 3 in person and one online trainings on Neurodiversity Affirming Practice for Mental Health, plus delivered a workshop at the OTNZ-WNA conference on Neurodiversity and Trauma-Informed Occupational Therapy and a training on Neurodiversity Affirming Practice for a group of local mental health occupational therapists for their study day.
It has been such a joy and an honour to deliver these trainings and as I look forward into this year and planning which trainings to do, I thought I would take the time to outline some of my thoughts on what I mean by neurodiversity affirming practice and an outline of some of the important concepts and ideas. Many of these concepts and ideas are big and I cannot possibly do them justice here, this is meant to be a quick taster. I will also give some links to where you can find more information. I was trying to get this finished in January, but here we are in May and at last I’m getting there.
Image descriptions - 1: Live in person training in Canberra June, 2024. Picture shows title slide for ‘Neurodiversity Affirming Practice’ up on a screen. A table with a laptop, water bottle and other resources is also visible below the screen. 2: a picture of myself, a brown-haired person wearing blue glasses, smiling and holding up printed copies of the handout and slides for the neurodiversity affirming practice training. 3: Online training August 2024. Picture shows title slide for ‘Neurodiversity Affirming Practice’ on a computer monitor with a laptop open and a microphone below. Many fidgets are on the table as well as paper copies of the slides. 4: Resource table for Mental Health OT study day, November 2024. Picture shows two boxes of sensory tools and fidgets, selected books related to neurodivergence, pens, paper, ND and Me cards and resources from Wildling Books.
Neurodiversity affirming vs neurodivergent affirming
Language in this space is important AND it is also continuing to evolve. I was wanting to clarify here why I am specifically using the term neurodiversity affirming practice rather than neurodivergent affirming practice. This is an intentional choice and not an error. First some definitions:
Neurodiversity - refers to the whole range of human brains, typical and divergent. Neurodiversity is a natural part of human diversity, think of it like biodiversity.
Neurodivergent - having a brain that functions differently and falls outside the social norms. This is a big umbrella that includes any way a brain diverges from ‘normal’ e.g. Autism, ADHD, mental health conditions, ‘personality disorders’ (I won’t open that can of worms here, but I do have some thoughts about these), brain injury, specific learning disorders (dyslexia, dyscalculia etc.) and many more.
(For more neurodiversity definitions I often refer people to Dr Nick Walker’s page where they define some key terms in a really clear way, with examples of correct and incorrect usage)
Therefore neurodiversity affirming practice is affirming of all types of brains which is why I am continuing to use this term. What I talk about are ways to adapt, accommodate, support and affirm all kinds of different brains, using universal design principles. I don’t often talk about specific supports for specific diagnostic labels as everyone is so different and needs different supports and the things I talk about can benefit all people, neurodivergent and neurotypical.
I have seen some people moving to using terms like neurodivergent affirming or neuro-affirming and will continue to watch the way the language is evolving and may change what I use in the future, but for now I am continuing to use neurodiversity affirming intentionally as it reflects what I am trying to do in improving supports and understanding for all types of brains across the whole range of neurodiversity.
Components of Neurodiversity Affirming Practice
Neurodiversity affirming practice is not (and cannot by definition be) a set recipe, it’s an ongoing reflective practice. I see my role as providing an introduction to useful frameworks, principles, important concepts and ideas, and additional resources, and it is then up to the individual to keep exploring, reflecting and changing their practice step by step. To continue the kitchen metaphor, it’s like teaching people general cooking skills, not giving a set recipe, as I don’t know the environment you’re cooking in or the ingredients you have to cook with.
I am continually learning and reflecting and will continue to do so and hope that you will too.
What follows is a brief outline of what I usually cover when I talk about neurodiversity affirming practice. It is not a recipe book. I cannot give you a list of ‘10 things that make you neurodiversity affirming’. There is no one set answer, but there are some concepts and principles that can help you discover what being neurodiversity-affirming looks like for you in your setting.
Image description: Contents slide outlining the different topics covered with my neurodiversity affirming practice trainings listed as dot points and colour coded.
Language and Definitions
I use identity first language (Autistic person) rather than person first language (person with Autism) to honour the preferences of a large majority of neurodivergent people (especially within the Autistic community). My neurodivergence isn’t with me, it is a core part of me. Other people will have different preferences, always check with the person.
Neurodivergent (ND) - Having a brain that functions differently and falls outside the social norm. Innate or acquired. Can be multiply neurodivergent
Neurodivergence - the state of being neurodivergent.
Multiply neurodivergent - a person whose neurocognitive functioning diverges in multiple ways – for instance, a person who is Autistic, dyslexic, and epileptic.
Neurotypical (NT) - brain functioning that falls within societal standards of “normal.”
Neurodiverse group - a group in which multiple neurocognitive styles are represented. There is no such thing as a “neurodiverse individual.” The correct term is “neurodivergent individual.” An individual can diverge, but an individual cannot be diverse.
Make it stand out
See above for my thoughts on neurodiversity-affirming vs neurodivergent affirming.
For more on definitions - Nick Walker https://neuroqueer.com/neurodiversity-terms-and-definitions/
Image description: blue text boxes on a tan background with neurodiversity terms and definitions. Also pictured is the neurodivergent umbrella with examples of different kinds of neurodivergence.
I also cover a range of other useful words to know (below) and how they might relate to practice/what you might see. I personally find it so affirming when I use a term and don’t have to explain it to a health professional I’m working with. I have also had positive feedback from clients when we’re talking about something and they use a term like masking and they can describe their experience without having to explain the concept.
Masking - hiding your true self to conform to societal expectations.
Stimming - repetitive movements of body or objects, often for self-regulation.
Pathological demand avoidance (Pervasive Drive for Autonomy, PDA) - reaction to and avoidance of demands (it is much deeper than this I know)
Interoception - the sense of the body’s internal states (hunger, thirst, emotions, etc.)
Executive functioning - set of cognitive processes that help us plan, reason and stay on task.
Synesthesia - experiencing sensations in more than one sense, e.g. seeing colours while listening to music.
Alexithymia - difficulty identifying, describing and expressing emotions.
Sensory modulation - changing how we feel using the senses.
Aphantasia - inability to picture things in your mind.
Monotropism - a mind that is pulled towards a single point of focus.
Misophonia - a strong reaction to specific sounds, reaction may appear ‘unreasonable’.
Rejection Sensitivity Dysphoria (RSD) - emotional pain from perceived failure or rejection.
Frameworks, principles and models
1. Core Principles of Neurodiversity Affirming Practice (Wise, 2023); 2. EMPOWER model (Carlson-Giving, 2023); 3. Raelene Dundon (2023); 4. The DIVERSE Model of Neurodivergent Affirming Practice (Peters, 2023)
These models have all been developed by those with lived experience and more will continue to come out. I also speak about recovery-oriented and trauma-informed practice as a key component of neurodiversity affirming practice and how many of the principles overlap.
I introduce these frameworks, not to go through them in detail but as a signpost to their existence. The focus is on the person finding a framework that suits their brain and setting, and then using that to support setting action steps for change.
Jennifer Kemp also has this great resource and checklist ‘Is Your Practice Neurodiversity Affirming?’. I did some training last year with her and she is also developing a framework for effective and affirming therapy, but it isn’t live and out there yet so I can’t share here.
This graphic from Newglade Counselling highlights the cycle where trauma occurs for neurodivergent people from being consistently misunderstood and not getting their needs met. Neurodivergent people are more likely to have experienced trauma, including this type of chronic invalidation, that can have a lasting impact. This is why it is vital to be trauma-informed while also being neurodiversity affirming in our practice when we are supporting neurodivergent people.
Image description: graphic by Amy Peters, Newglade Counselling of ‘The Neurodivergence Trauma Cycle’. Five different coloured circles with arrows between each: negative experience -> masking -> self-blame -> hypervigilance -> intensifying stress -> negative experience.
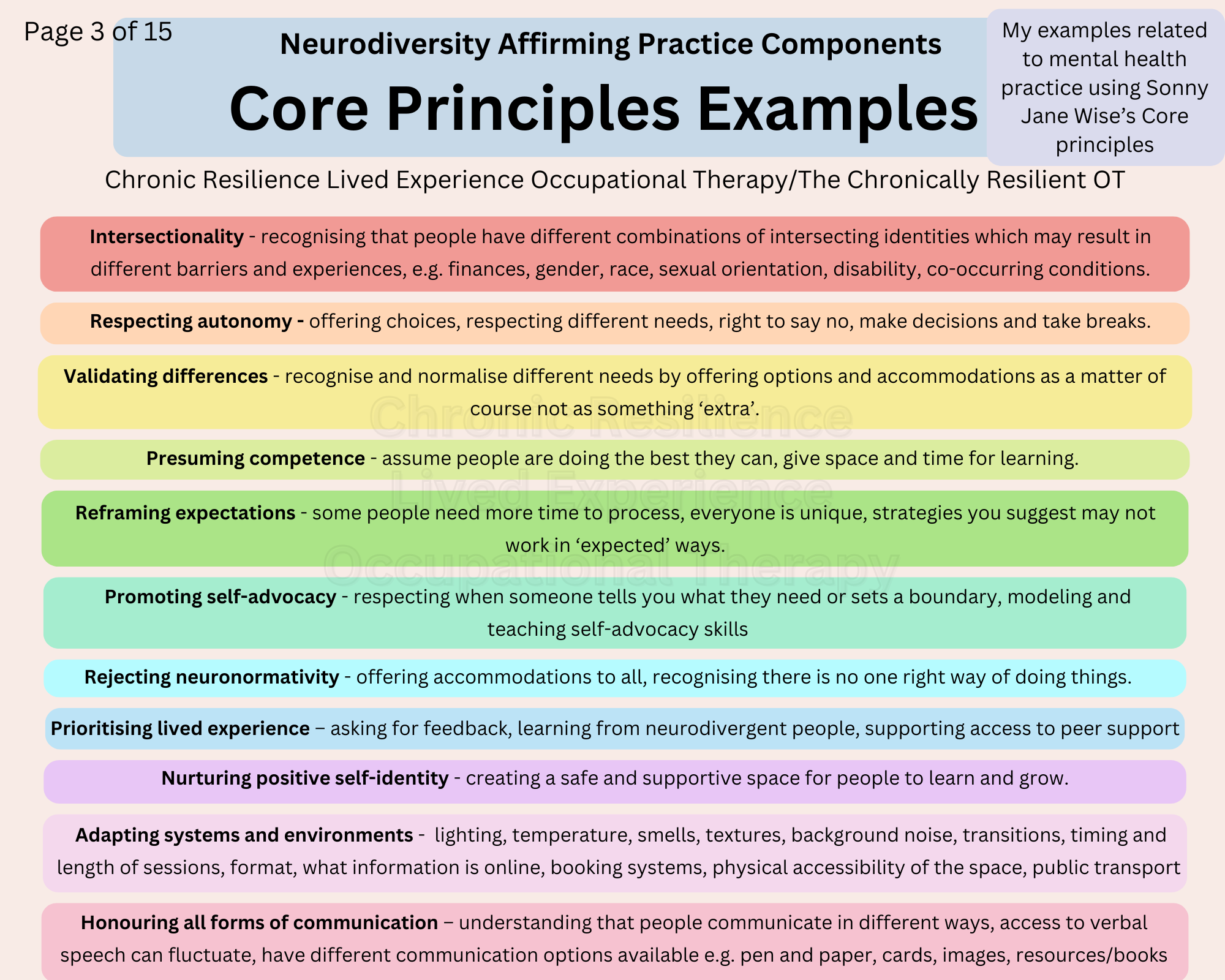
I use Sonny Jane Wise’s Neurodiversity Affirming Practice Core Principles as a framing and give my own examples related to mental health practice for each one. I also ask people to think about and note down things relevant to their own practice for each principle as a way of starting to think about what areas they might start to create change.
Image description: a series of different coloured boxes titled with a core principles of neurodiversity affirming practice with mental health related examples. Intersectionality - recognising that people have different combinations of intersecting identities which may result in different barriers and experiences, e.g. finances, gender, race, sexual orientation, disability, co-occurring conditions. Respecting autonomy - offering choices, respecting different needs, right to say no, make decisions and take breaks. Validating differences - recognise and normalise different needs by offering options and accommodations as a matter of course not as something ‘extra’. Presuming competence - assume people are doing the best they can, give space and time for learning. Reframing expectations - some people need more time to process, everyone is unique, strategies you suggest may not work in ‘expected’ ways. Promoting self-advocacy - respecting when someone tells you what they need or sets a boundary, modeling and teaching self-advocacy skills. Rejecting neuronormativity - offering accommodations to all, recognising there is no one right way of doing things. Prioritising lived experience – asking for feedback, learning from neurodivergent people, supporting access to peer support. Nurturing positive self-identity - creating a safe and supportive space for people to learn and grow. Adapting systems and environments - lighting, temperature, smells, textures, background noise, transitions, timing and length of sessions, format, what information is online, booking systems, physical accessibility of the space, public transport. Honouring all forms of communication – understanding that people communicate in different ways, access to verbal speech can fluctuate, have different communication options available e.g. pen and paper, cards, images, resources/books.
Medical and Social Model of Disability
With the medical model of disability the problem is with the person, it is very deficit focused and can often feel like it is blaming the individual.
A better framing is to use the social model of disability where disability occurs because of barriers in the environment and society around the individual.
Image description: coloured text boxes on tan background defining the medical and social models of disability. Next to the medical model description is an outline of a person with arrows pointing towards them and the word ‘problem’ inside. Next to the social model description there is an outline of a person, the arrows point away from the person and the word ‘problem’ is outside them.
Alexithymia and Interoception
These two have their own sections as they are such important concepts to understand and support as they can influence the efficacy of supports and interventions we might be providing. For example, it’s difficult to learn emotion regulation skills if you aren’t aware of signals from your body (interoception) or if you have difficulty Identifying, differentiating, describing and verbally expressing feelings (alexithymia). We may need to work at a more foundational level to improve interoceptive awareness - doing this very slowly and gently - and/or working with someone to find other ways to identify and express their emotions.
Image descriptions: black text on tan background describing Alexithymia and Interoception. 1: With Alexithymia a person might... Have difficulty Identifying, differentiating, describing and verbally expressing feelings; Struggle to tell the difference between bodily signals and emotions (e.g. anxious or hungry?).; Have unexpected reactions or not express emotions in a ‘typical’ fashion; Rely on physical sensations to triangulate emotions → Need additional tools for supporting connection with emotions and learning different ways to understand and describe their experiences. Important note: this is not about teaching someone to mask or teaching ‘typical’ emotional expression. It is about supporting a person to explore what emotions look and feel like for them and building trust in their internal experience, which may include reconnecting to their bodies and trauma processing. Image of series of sloths saying ‘on a scale of sloths how do you feel today?’. 2: Interoception: our body’s internal sense. Receptors in the body send signals to the brain to let us know what we need (body needs and emotions). Low interoceptive awareness: people may have difficulty responding to their needs as they might not know when they’re hungry, full, thirsty, sleepy, unwell, recognise early signs of distress or be able to identify emotions. High interoceptive awareness: might be acutely sensitive to their internal experiences and have low tolerance to uncomfortable sensations, may appear to ‘overreact’ or be called ‘sensitive’. Interoceptive awareness can be improved by slowly and gently increasing awareness of what’s happening internally (being trauma-sensitive always). Some people may always need external cues e.g. a timer to eat. Note: any exercises are not about exposure to distressing sensations or desensitising, they are always done collaboratively at the right pace for the person. Image from Kelly Mahler of an outline of a person and all the body systems around the outside.
Sensory Processing
I have a whole training on sensory processing as I feel it is so foundational to our work in mental health and it’s a special interest area of mine. I also have a separate blog and worksheet on the topic.
Everything we do and experience has a sensory component and everybody has their own unique way of processing sensory information.
Sensory processing refers to how we take in information through the eight senses (external and internal information), organise and interpret the information and use it to interact with the environment.
There are many sensory related things that can be adjusted, adapted and changed and they are often the low hanging fruit and an easy place to start when you’re making a shift to being more neurodiversity affirming. One of the keys here is as much as possible have spaces with adjustable sensory inputs so you can accommodate people with different sensory processing patterns and needs.
Below I have broken down some of the sensory related things to be aware ok, look out for or change:
Auditory - Background noise, humming of lights/fans/electricity, your speaking volume, auditory processing speed
Visual (sight) - Visual clutter in the space, unexpected changes, colours, artwork, clear pathways, information, signage, resources
Gustatory (taste) - Mindfulness practices using food, grounding and anti-dissociative resources, preferences
Olfactory (smell) - Diffusers, essential oils, candles, soaps, perfumes, cleaning products
Vestibular - May seek out additional input and need to move around during a session or sit in different positions
Proprioception - Sense of body in space, body map, awareness/lack of may impact capacity to stay focused
Interoception - Internal body sense, hyper or hypo awareness of emotions or sensations, tension, breathing; links to alexithymia and emotion regulation
Tactile (touch) - Seats, blankets, cushions, fidgets, the use of touch (with consent and as appropriate depending on your modality)
Communication
People communicate in many different ways and may need different strategies or supports at different times, e.g. if people are situationally mute. Communication can also be supported by managing vulnerabilities and supporting mental health more generally. Learning to understand and then communicate your needs is a key skill and you may work with someone on building their self-advocacy skills too.
Two key concepts in this section:
The Double Empathy Problem (Milton, 2012) - The mismatch between two people that can lead to faulty communication. It is easier to empathise with people you relate to and are neurologically wired like, e.g. allistic (non-autistic) people communicate better with allistic people, autistic people communicate better with other autistic people. Communication breakdown occurs when you mix the different styles, e.g. different meanings for eye contact, can still be paying attention when looking away or fidgeting, etc.
The Triple Empathy Problem (Shaw, et al., 2023) - Cumulative disadvantage between a non-autistic health professional and an autistic patient where there is layered miscommunication potential beyond that of the double empathy problem. When I learned about this concept I wanted to shout it from the rooftops and it continues to be a real aha moment each time I do this training.
These have both been researched specifically with Autistic people, but I can see how the concept can extrapolate out to other types of neurodivergence.
Communication, The Double Empathy Problem and The Triple Empathy Problem
Image description: blue text box heading ‘Communication’, with the following text: People communicate in many different ways and may need different strategies or supports at different times, e.g. communication cards, verbal speech, writing. Communication and interaction styles vary by culture, belief, gender, societal traditions and expectations, age, generation, personality, neurodivergence, etc. Things to consider in practice: Differences in use of eye contact, understanding indirect language (sarcasm) or body language; The Double Empathy Problem (Damien Milton, 2012) and The Triple Empathy Problem (Shaw, et al., 2023); Need for clear, direct instructions, be aware of how you communicate and check for understanding; Multimodal communication e.g. verbally explaining something as well as giving written information. Graphic representation of the double and triple empathy problem.
Co-occurring conditions
There are high rates of co-occurring physical and mental health conditions in neurodivergent populations. Many people also have combinations of different types of neurodivergence e.g. Autism + ADHD + Dyslexia, Autism + OCD.
In one study 86.8% of Autistic adults reported a psychiatric or behavioural condition, 52.8% had three or more diagnoses (Jadav & Bal, 2022).
Neurodivergent participants had higher prevalence of hypermobility (51% - general population 20%) and reported significantly more orthostatic intolerance and musculoskeletal pain (Csecs, et al., 2022).
Resource: ‘All The Things’ from All Brains Belong (2024), looks at the overlaps of different health conditions and aims to improve the healthcare of Autistic and ADHD adults by improving knowledge and educating health professionals. It’s a great place to start.
Co-occurring conditions and experiences can have a big impact on treatment modalities and strategies, e.g. advice for ADHD is to use intense exercise as a management strategy but if someone has a fatigue condition they won’t be able to do this.
Co-Occurring Conditions - overlap is the rule, not the exception
Always consider what else might be going on for someone.
Image description: blue text box heading ‘Co-Occurring Conditions’, with the following text: Many people have combinations of different types of neurodivergence e.g. Autism + ADHD + Dyslexia, Autism + OCD. Look for different kinds of neurodivergence as well as chronic illnesses, hypermobility and pain conditions which occur more frequently in neurodivergent populations. Consider how you can support and accommodate different needs: Impact of symptoms/experiences on participation in meaningful activities and the impact on mental health; Session length and timing, online options, seating; Symptoms can impact follow through of strategies; Trauma-informed practice, creating safety, clear instructions, consent, predictability and familiarity.
Missed and misdiagnosis
When I first added this section into the training, it turned out to be a bigger section that I had anticipated. There has been, and still is, so much missed and misdiagnosis and it has a big impact on people. I think my favourite sentence to write and say has been “If someone has had depression and anxiety for 20 years, it’s probably something else.” We need to do better and look deeper. Things are shifting, and we still have a long way to go.
I highly recommend Dr Neff’s resources, especially the Neurodivergent Insights Misdiagnosis Monday series of venn diagrams for some great overviews of how different types of neurodivergence overlap and where the differences are.
Dr Neff on Autism, BPD and ADHD: “All three conditions share genetic, temperamental, and trait overlap. They also share many psycho-social risks, such as victimization, substance abuse, disordered eating, mood disorders, PTSD, self-harm, and more. Even among seasoned clinicians who know these conditions well, it can be incredibly difficult to differentiate and spot the differences.” (Neff, 2023)
High rates of, and gender differences with, missed and misdiagnosis.
Image description: blue text box heading ‘Missed and misdiagnosis’. Three different coloured text boxes with arrows connecting them, from left to right: Underdiagnosis, Misdiagnosis, Late disagnosis or late realisation -> Delays in self understanding and support, Lack of, or inappropriate, support -> Trauma, Chronic invalidation, Masking, Gaslighting, Burnout, Addiction, Suicidality, Reduced QoL. Below this: In practice: Look out for other things that might be going on as it is likely to be more than just one thing; Consider previous negative experiences and always be trauma sensitive; If someone has had depression and anxiety for 20 years, it’s probably something else.
Support and accommodations
As an occupational therapist, this section is really at the heart of what I do. It’s practical, and appropriate support and accommodations make such a massive difference to people.
Using the PEO model (below, left), when the person, their environment and their occupation are aligned we get good occupational performance. When there is a mismatch we need accommodations to improve the fit. In neurodiversity affirming practice it’s more about adapting the environment and modifying the task than changing the person (unless skill development is a person driven goal and is done in an affirming way).
We need to also consider
Fluctuating capacity, functioning and skill so may need different levels of support on different days - this can be challenging for the individual and those around them to understand.
Spiky profiles - People have areas of skills and strengths and other areas where they need supports and accommodations. So maybe someone can go to work but they can’t cook for themselves and need additional support in that area.
We also know that some simple changes and accommodations can make a big difference (below, right). There’s a few versions of this accommodations graphic now (there’s a worksheet and downloadable graphics available), it was one of my first and continues to make an impact around the world. It illustrates how a person can get to overwhelm by a cumulation of many factors, and by changing the things we can change, many of these factors now have less impact and the person has more capacity to engage in therapy.
Supports and accommodations will look different for each person. I bring in Universal Design Principles as well, as if we can design for most and then make individual accommodations as needed, we can ensure we are providing affirming support to as many people as possible - while also taking our own needs and accommodations into account.
Image descriptions: blue text box headings with tan background.
Left: ‘Support and Accommodations’ Three overlapping circles: person, environment and occupation with an arrow pointing to the area of overlap in the centre labelled ‘PEO components overlap to create occupational performance - the doing’. More overlap = better performance. This will shift and change across the lifespan and depending on the task and the environment. PEO mismatch. The three circles are no longer overlapping, the environment and occupation circles have shifted towards the edges of the graphic, arrows under the words indicate the need for movement. Need accommodations to improve the fit. Adapt the environment + modify the task = improved occupational performance. Below this: In neurodiversity affirming practice it’s more about adapting the environment and modifying the task than changing the person (unless skill development is a person driven goal and is done in an affirming way). Also consider: Fluctuating capacity, functioning and skill so may need different levels of support on different days; Spiky profiles - People have areas of skills and strengths and other areas where they need supports and accommodations.
Right: ‘Accommodations Make A Difference’ . a 3 panel comic with a brown background. The heading reads ‘Accommodations make a difference’, below the heading text says ‘The ability to engage in something like a mental health appointment can be impacted by many factors. On any given day, the combination that results in overload can be different. Simple accommodations can increase someone's capacity and ability to participate and engage. The first panel has a scale from 0-100 with different coloured boxes from green at the bottom to red at the top. The top box sits on top about to fill up the scale to 100 – the box says ‘therapist going away.’ Above this text says: One more task demand or something unexpected could result in overwhelm/meltdown for this person. Middle panel: a bulleted list says ‘What could you change? Quiet waiting room, Online booking options, Various seating options, No perfume, Check noise levels in room with client, turn off fans etc., Affirming approach, validation and acceptance of the person. Below this are some of the coloured boxes from the first panel all smaller with a spiky circle that says ‘these factors now have less impact.’ Third panel: text at the top says ‘With accommodations in place, the same demand, 'therapist going away', doesn't have the same impact.’ This is the difference simple accommodations can make. There is the 0-100 scale but now only 3 boxes are filled in, a yellow box fits on top and doesn’t cause overwhelm – this is the difference simple accommodations can make.
Lived experience feedback
It was really important to me that I get more lived experience feedback than just my own to include in this training, so I asked some questions in a range of neurodivergent facebook groups, got some wonderful responses and summarised them to include in the training.
For more detail on this there is a related blog and free resource. I will also be presenting the results at a conference later this year.
Image descriptions: blue text box headings with tan background.
Left: ‘Lived Experience Feedback’ Barriers to accessing/receiving mental health supports (in different coloured text boxes): Dismissal, invalidation, lack of knowledge, outdated ideas; Lack of understanding of different communication needs; Double empathy problem, misinterpretations, assumptions, not taking things seriously if the nonverbal cues don’t match content; Claiming expertise then not delivering; Lack of understanding from family and other supports; Not adapting approach to support neurodivergent brains e.g. mindfulness; Overuse of CBT as a modality, harmful nature of some evidence based practices; Misinterpreting executive functioning difficulties as a lack of motivation, not trying hard enough or ‘non-compliance’; Not understanding environmental barriers or the social model of disability; Previous negative experiences, not knowing when to seek help or where to go; Misdiagnosis impacting subsequent treatment, inappropriate crisis responses; Cost, funding systems, location, transport, parking, sensory input; Racism, sexism, transphobia, misogyny, ableism, stigma; The number of steps it takes to get help, having to make phone calls.
Right: ‘Lived Experience Feedback’ Things that help (grouped into 6 categories inside different coloured text boxes with a related symbol): Therapist characteristices - Shared experiences, honesty, compassion, authenticity, genuineness, caring, respect, kindness, curiosity, validating, non-judgemental; Approach - Boundaries, cooperative model of care, direct communication, be ok with tangents, understand the real difficulties, respecting where the person is at; Knowledge - Trauma-informed, neurodiversity affirming, understanding of co-occurring conditions and misdiagnosis, intersectionality and gender diversity; Session Adaptations - Multimodal approaches, adaptations to modalities, different locations, movement, online or phone option; Communication - Alternatives to phone calls, reminders, accountability check ins, current photo and bio, clear forms; Accommodations - Freedom to fidget and stim, sit in preferred position, alternatives to emotion words and visualisation practices, executive functioning supports, quiet spaces, adjustable sensory inputs.
Final Thoughts
When thinking about what it all boils down to, For me neurodiversity affirming practice comes down to: Ask, Listen, Be curious, Validate.
Image description: 4 different coloured boxes each with one of the following words and an image from left to right: Ask (question mark), Listen (ear), Be curious (magnifying glass), Validate (hand with heart).
As I said at the beginning, it is an ongoing reflective practice, not a box you tick once and never look at again. I encourage you to have a look at your own practice and reflect on:
What’s going well?
What will you start to do differently to be more neurodiversity affirming?
What is actually possible in your setting?
What is one action step you can take next week? (Keep it simple and specific)
Who could you connect with to discuss these concepts further and get support from?
I am working on getting the recordings of my Neurodiversity Affirming Practice training up on the website as an on demand course but have hit some tech barriers and need to revisit it once some upcoming projects are out of the way.
For upcoming events - they will be listed here.
I always try to signpost to additional resources and have compiled a non-exhaustive list here.
Note: when looking for information prioritise lived experience voices, seek out different intersectionalities of identity e.g. non-speaking, BIPOC, trans etc.; avoid anywhere that uses the puzzle piece symbol or talks about ‘curing’ or encouraging masking, especially for Autism.
Pages/People: Neurowild, Embrace the Muchness, Reframing Autism, Yellow Ladybugs, Autism Level UP, The Lived Experience Educator, Neurodivergent Insights, Dr Alice Nicholls, Kelly Mahler - interoception, Sensory Modulation Brisbane, How To ADHD, Ben B. - "My Own Words: Reflections of a Non-Speaking Autistic”, The Hypermobility MD, Dr Bendy Brain - Dr Jessica Eccles, Autistic Doctor’s International, All Brains Belong.
Podcasts: Divergent Conversations, The Neurodivergent Woman, Square Peg, The POTScast, The Rest Room, Two Sides of the Spectrum, and many more...
Books: Neuroqueer Heresies by Nick Walker, Unmasking Autism by Dr Devon Price, Different Not Less by Chloe Hayden, What I Mean When I Say I’m Autistic by Annie Kotowicz, I Am Autistic and This Is ADHD by Chanelle Moriah, Still Distracted After All These Years by Kathleen Nadeau, A Day With No Words by Tiffany Hammond, The Rainbow Brain and The Brain Forest by Sandhya Menon, Wild Of Brain by Anissa Ljanta, and so many more...
For more on books, I keep a reading list record and review what I’ve been reading on this page.